Evidence of Brain Activity in the Early Stages of Chronic Pain from a Patient’s Theoretical Diagnosis and Clinical Trials
“You have to give each drug at least six weeks to see if it works, before trying the next one,” Russo says. Each drug can cause side effects, whether or not it eases the pain. After cycling through each migraine drug individually, the team started testing drug combinations. “We finally got control of her migraines on the 24th medication trial,” Russo says.
There are many different types of non-opioid drugs that have pain-relieving (anagelsic) benefits as well as a number of other non-pharmaceutical options for chronic pain relief. But the guesswork means that chronic pain care is still a highly frustrating process for patients and clinicians, says Sean Mackey, a physician–researcher in pain medicine at Stanford University in California. “The issue is not that we’re short of quality pain treatments,” Mackey says. “The issue is that we don’t know how to match them up to the right patient.”
These human complexities make efforts to capture pain in the brain difficult, let alone being able to identify biomarkers that would guide physicians to the best treatment for each person. Carl Saab, founder and scientific director at the Cleveland Clinic Consortium for Pain in Ohio, says that there can be some correlation between pain and brain activity. The signal that pain is preserved in mammals and non-human primates is very clear. The pain sufferers have different diagnoses of the brain activity in their eyes. “Pain is one of the most heterogeneous clinical conditions I know,” says Saab. “Your pain is different than mine, because your approach to life is different — you might worry about your family more than me, or your job — and so when I average you with 50 other people, that signal is going to get washed out.”
It is possible for an optimistic person who breaks an arm mountain biking on a weekend away with friends to experience pain differently than a pessimist who is behind on their mortgage repayments. It can be possible to have anxiety and depression that lead to chronic pain. “Nobody experiencing chronic pain is in the same place at the same time,” she says. Everything else around them, everything they have already experienced, everything they are anticipating, and all the emotions that arise from that experience, constitute the context of that pain.
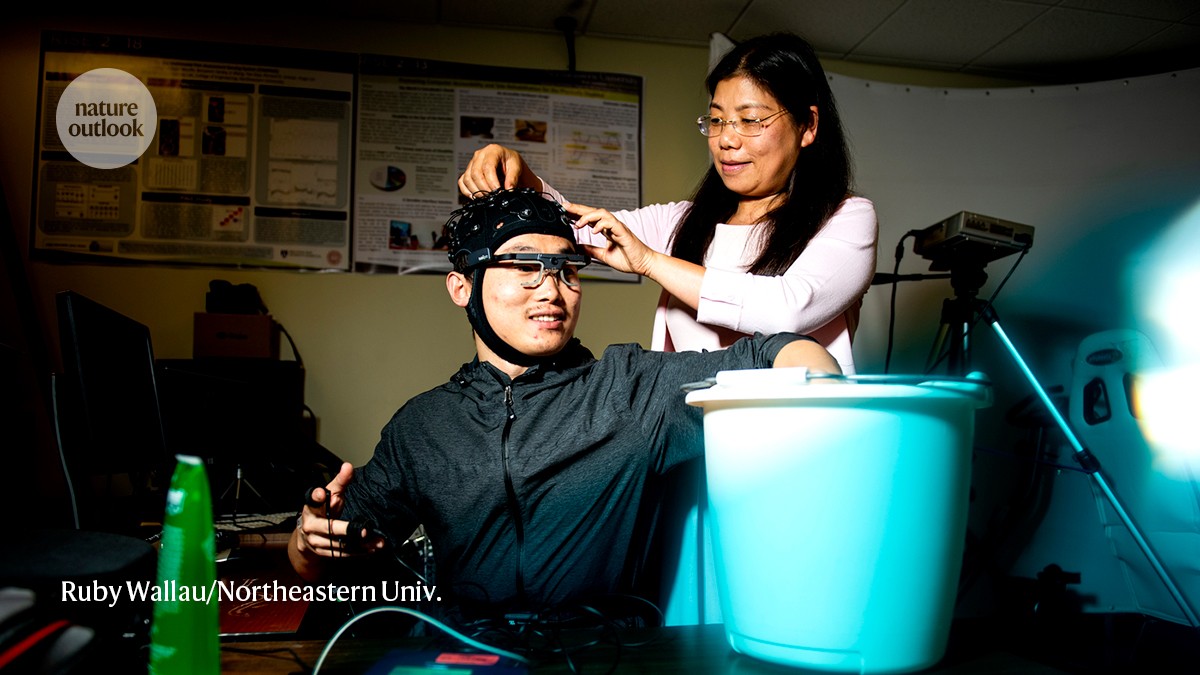
EEG phenotyping of chronic back pain using an artificial intelligence algorithm inspired by Saab’s experiment with a structural brain marker
It made it into the human eye. “When we compared the EEGs of people with pain versus those with no pain, standard statistical analysis showed no difference,” Saab says. When Saab and his collaborators trialled a basic form of machine learning to process the data, however, the artificial intelligence (AI) algorithm could detect something. There was a difference between those with chronic back pain and healthy people, but also between those who would benefit from a stimulator and those who wouldn’t. The algorithm had an of accuracy almost 80%, Saab says, showing that even a simple AI can outperform conventional statistics for the task. “Basic machine learning is picking up signals that classic methods and the human eye are not capable of detecting.”
Vollert has seen similar results from applying basic machine learning to an approach called sensory phenotyping. He has used this technique with people experiencing neuropathic pain, which arises from nerve damage. The idea is to assess the broad changes to the sensory system that typically accompany pain. Vollert says many people get sensitized to sounds or smells with a strong headaches.
The early results were promising. “In 2012, when I first published work using structural brain imaging to classify the presence or absence of lower back pain, we got 76% accuracy,” says Mackey5. Progress then stalled. “Since then, the accuracy hasn’t got much better,” he says.
By pooling data from multiple biomarker techniques, however, a stronger signal should emerge. “Where the field is going is to bring all these data sets together,” says Vollert, who is currently participating in two such efforts in Europe: the IMI-PainCare Biopain consortium led by Rolf-Detlef Treede, a neuroscientist at the University of Heidelberg in Mannheim, Germany, and Painstorm, led by David Bennett, a neurologist at the University of Oxford, UK. Prospective data sets that collect all kinds of marker information in parallel from the same patients are needed to build really good models. “That’s the kind of data set that we’re generating at the moment.”
Vollert believes that advanced artificial intelligence tools will be vital to categorizing people into groups and treatment groups with multimodal data. He says they are trying to find models that can go deeper into the data.
Preliminary findings suggest that advanced deep-learning AI could be transformative for accurate pain biomarker identification, says Mackey. We recently used some really advanced artificial intelligence techniques on data from a highly heterogeneous population, and we were able to get classification accuracy around 90%. The next step is to link treatment outcomes to the ability to accurately and objectively classify people with pain into subgroup.
One caveat is that these advanced AI techniques apply non-interpretable models to biomarker data analysis. “In my early work with machine learning, I could tell you exactly what brain regions were contributing to the model,” says Mackey. We can get great accuracy with the new and improved versions, but I can not say what is driving it.
Non-interpretable modelling presents a problem for pain-medicine practitioners, Mackey says. “As clinicians, we want to understand the basis of a medical recommendation and not just blindly take the word of a machine — because what if the machine is wrong?”
After coming under Russo’s care, it took three long years to find a way to control her migraines. The problem was not a shortage of options — there are plenty of treatments for people with chronic migraines, Russo says. Trying one treatment at a time for a person with chronic pain can be difficult in hopes of finding a match.
Her migraines would often be on a daily schedule. A pain-medicine physician at Hunter Pain Specialists in Broadmeadow, Australia, who treated her in consultation with a neurologist, says that she vomited and had to lie down. “Then she’d have to get up, rinse her mouth and see the next patient.”
I’m not sure what I should do about it. Pain assessment and sensor learning can improve the effectiveness of pain management if you can communicate your symptoms
“Hmm, it’s not really working,” says Lin, acknowledging that much optimization work remains. Maybe we should stop. When I take my hand out of the cold, the pain is gone in a few moments, and I don’t need an objective measure to know when it is gone.
The platform proved to be glitchy. The pain scores displayed on the app went up as I submerged my hand in ice water. The readings were inconsistent, however, fluctuating as I experienced a steadily increasing sensation of pain.
When I tried the cold-exposure task in her lab, I had just one sensor on my body. Facial tracking, measurements of pupil diameter and monitoring of brain activity weren’t recorded.
The researchers found in a study of cold-inducing pain that a model derived from facial expressions and brain activity was better than a more limited set of indicators. The front. Neurosci. 16, 831627; 2022).
Lin has been fine-tuning her platform called Continuous Objective Multimodal Pain Assessment Sensing System (COMPASS) using data from people with chronic low back pain to validate her group’s machine-learning algorithms. Artificial-intelligence tools have been able to synthesise diverse data sets to extract valuable insights that align with people’s own pain assessments.
A snapshot of pain is provided by the technology of AlgometRx. That is fine for some situations, such as an assessment by a physician, but it can’t track the variation in pain levels over time.
But the cost and complexity of brain-recording technologies make these methods unsuitable for clinical use. “It has to be practical and portable,” Saab says — which is where simpler diagnostic tools and wearable devices come in.
In the US, the platform can be used during surgery with people who are unable to communicate their pain levels. It aims to modify the dosages of the drugs in order to maximize pain management and reduce the risks of unnecessary prescriptions.
Moreover, many individuals — including babies, people who are non-verbal, people who are critically injured and those under sedation — cannot communicate their symptoms effectively. This makes it difficult to manage pain and hinders the delivery of appropriate analgesia.
As discomfort escalates to pain, a sensor strapped to my chest detects changes in my heart rate, breathing pattern, skin conductance and other bodily responses. These physiological signals are processed through advanced algorithms to generate a pain score. Displayed on a smartphone app, my pain level is 4.
The graduate student bears down on my arm with a force akin to a firm handshake. The sensation starts to get hurt when concentrated on a patch of skin smaller than a small coin.