T-cell cancer therapies based on the formation and response of a patient’s immune system to an invader’s own T cells
The researchers began by separating T cells from the blood of 16 patients with solid tumors, including colon, breast, or lung cancer. (T cells are the immune system component with these receptors.) They identified dozens of receptors that can bind to cancer cells taken from patients’ tumors. The team chose up to 3receptors for each patient, and added genes for them to their T cells in the lab.
The chief scientific officer of Pact has an author on the study. The company worked with experts from the University of California, Los Angeles, the California Institute of Technology, and the nonprofit Institute for Systems Biology in Seattle to design the personalized therapies.
Although the efficacy of the treatment was low, the researchers used relatively small doses of T cells to establish the safety of the approach, says Ribas. “We just need to hit it stronger the next time,” he says.
The patients’ cancers were already very advanced by the time they were part of the trial, and Mandl suspected that the response to the therapy was limited. Also, later tests revealed that some of the receptors the team chose could find the tumor, but didn’t have potent anticancer effects.
“It is probably the most complicated therapy ever attempted in the clinic,” says study co-author Antoni Ribas, a cancer researcher and physician at the University of California, Los Angeles. We want to convert a patient’s own T cells into an army.
The researchers used the predictions from the data to make a model to predict which type of T cells might respond to the deletion of one of the genes. The lead author of the study says that if T cells can see something that isn’t normal, they kill it. “But in the patients we see in the clinic with cancer, at some point the immune system kind of lost the battle and the tumour grew.”
“This is a tremendously complicated manufacturing process,” says Joseph Fraietta, who designs T-cell cancer therapies at the University of Pennsylvania in Philadelphia. The entire procedure can take more than a year.
As researchers try to speed up the development of therapies, engineered cells will be cultured less and they will be more active. “The technology will get better and better,” says Fraietta.
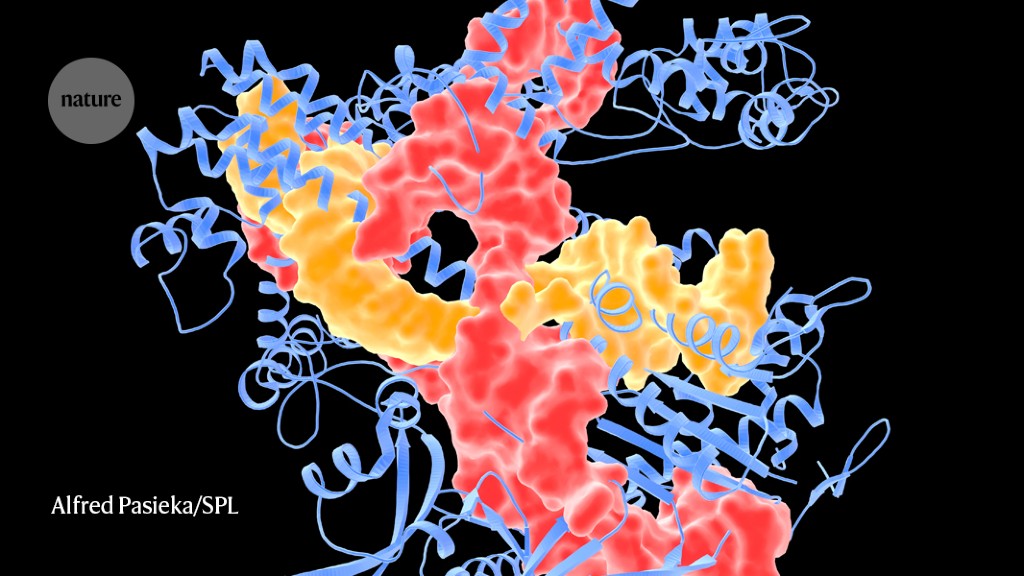
Elaborately engineered immune cells can not only recognize cancer cells, but also evade defences that tumours use to fend off attacks, researchers have found.
Fraietta says that the common surface proteins has not been found in solid tumours. And solid tumours provide physical barriers to T cells, which must circulate through the blood, travel to the tumour and then infiltrate it to kill the cancer cells. Tumour cells are known to suppress the immune system by releasing chemical signals and by using up the local supply of vitamins to fuel their rapid growth.
Controlling T-cell exhaustion using wired genetic circuits with IL-2 protein and gene-coded CAR microsatellite
It was approved to treat leukaemias, lymphomas and myelomas. But researchers have been pursuing ways to make the treatments safer and more effective, and to expand their use to other diseases.
A synthetic biologist at Boston University and his colleagues wired a system of 11 DNA sequence into CAR T cells. The resulting genetic circuits can be switched on and off using already-approved drugs, which allows researchers to control when and where the hacked T cells are active, as well as their production of a protein called IL-2 which stimulates immune responses.
T-cell exhaustion is a phenomenon when T cells become inactive after a long period of stimulation, and the ability to turn the T cells on and off may be able to help reduce it. Some studies have found that giving T cells a ‘rest period’ can reduce T cell exhaustion and boost their overall effectiveness against tumours3.